The universe has been trying to get me off this planet for years.
February 2015: It’s a cold Wednesday night and my Advanced Screenwriting Class (where undergraduate students complete a feature film script in one semester) has just wrapped up a scene-by-scene deconstruction of the iconic film Die Hard, which every aspiring screenwriter needs to study line-by-line. These are good kids—dedicated, disciplined, talented. You don’t sign up for a class like this unless you’re committed.
I’m in my twentieth year of teaching screenwriting at Tennessee’s first film school: The Watkins Film School, a division of the Watkins College of Art. I love teaching, but the college is dying. Our enrollment has been dropping steadily, semester after semester. Despite hefty annual increases in tuition, faculty and staff haven’t seen raises in years. Before it’s over, I’ll be assigned classes I’ve never taught before on subjects I know nothing about because we can’t afford to hire adjuncts who know what they’re doing.
It’s 8:30 or so on a frigid night and I head back to my office. I’m in no hurry to get home; my marriage has been deteriorating for a long time. My home life is not good. My faculty office is where I can get a little peace and quiet, especially late at night.
I turn to a stack of Intro Screenwriting student scripts and start marking them up. But suddenly, I feel really awful.
Truth is, I’ve been feeling lousy for months. I drive to work and the three-minute walk from the parking lot to my office leaves me panting. I have to sit down and get my breath before I start my classes. My energy levels are the lowest they’ve ever been. Earlier, I’d served a five-year term as Chair of the Watkins Film School, where I routinely put in fifty and sixty-hour weeks.
Now I was lucky to make my classes.
I put it off to stress and age. My personal life had been a raging dumpster fire for a decade-and-a-half. I became a parent for the first time at 48 (in a second marriage that failed after a decade), which is why I took the full-time teaching position. We needed the benefits and the regular paycheck. I mistakenly thought I could continue my writing career, that teaching wouldn’t be that demanding.
I was wrong.
In the decade before becoming a full-time college professor, I published nine novels. In the fifteen years after, I only published two. I was tired, stressed and depressed. I worked too hard, drank too much, and now I felt like hell.
On this February night, it got even worse. I was sick at my stomach and felt like somebody was sitting on my chest. I grabbed my coat and backpack, shut down my office and started the twenty mile drive to my house in West Nashville.
Once home, I kicked off my hikers, dropped my coat and backpack, then went straight to my bedroom. A few minutes later, my wife flicked on the bedroom light.
“What are you doing?” she asked.
“I’m tired,” I said. “Just thought I’d lay down for a minute.”
She came over to the bed and looked down at me. “No, you’re not.”
“What do you mean?” I said, cranky now. “Leave me alone.”
“Get your ass out of that bed,” she said. “We’re going to the hospital. I’m calling Bruce.”
My wife and Bruce, her primary care physician, had been close friends for decades, close enough that she had his private cell phone number. A couple of minutes go by and she walks back into the bedroom with a handful of aspirin.
“Bruce says put these under your tongue and call an ambulance.”
We both broke out laughing. My employer-provided health insurance was a joke—a high-deductible plan that covered almost nothing and cost nearly a grand a month. There was no way we could afford an ambulance.
“C’mon,” she said. “I can get you to the emergency room faster than an ambulance can get here anyway.”
A few hours later, I checked into a room at St. Thomas West in Nashville and was sucked into the black hole of the American health care medical/industrial complex. The blood draws, tests, scans quickly become a blur.
A day later, a cardiac team is standing at the foot of my bed giving me the results: five blocked arteries, including the infamous “widowmaker,” which was something like 80 percent closed. A doctor I’ve never met is telling me I need a quintuple cardiac bypass.
Quintuple bypass? I’d never even heard of that. Hey, go big or go home.
I begged for an alternative. I had too much to do; it was the middle of the semester.
“Can’t you give me meds and send me home?”
“Sure,” the cardiologist said. “We can give you meds and send you home to die.”
The surgery was delayed because an ice storm had hit the whole area. Staff and doctors couldn’t get to work. Four days later, I go under, not knowing if I’d wake up. The worst part was because of the ice storm, my ex-wife had been unable to get our two daughters to the hospital before the surgery.
I didn’t know if I’d ever see them again.
Fall 2018: I survived the quintuple bypass, entered a cardiac rehab program, passed with flying colors. I lost 25 pounds, even though I only topped out at 170 on my heaviest days, and was trying to get more exercise. I quit drinking completely for a year-and-a-half after the surgery, but the night Donald Trump beat Hilary Clinton, I turned to my wife and stepdaughter:
“I’m going to the wine store. I’ll be back.”
The stress levels are still high at work. It’s clear the college is going under. During my years as Chair of the Film School, our peak student body count was 167—by far the largest department in the college.
Now we were down to maybe thirty students or so.
A few years earlier, I’d applied for other teaching jobs, but faculty jobs in higher ed are harder than ever to get, especially in esoteric niches like film. I applied for about 25 openings and never got an interview. I was in my sixties now; it just wasn’t going to happen.
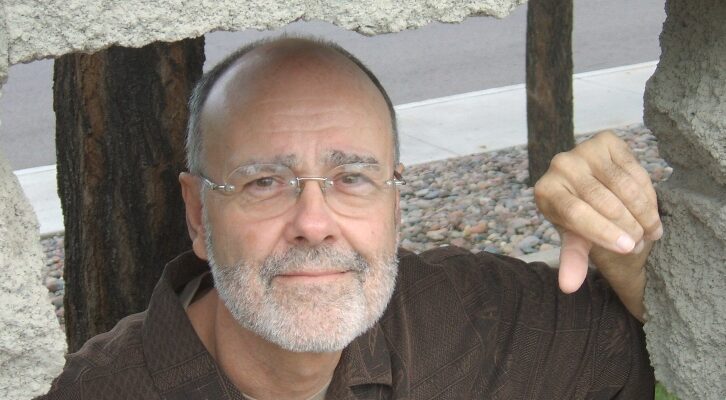
I began to contemplate a return to full-time writing. My most successful books, by far, had been a series of six private detective novels set in Nashville. I’d been nominated for an Edgar twice, won it once. Multiply nominated for the Shamus Award, I had one of those on my office bookshelf as well. The books had been under continuous option for film and TV rights since they were published up until the last few years, but nothing ever came of it.
Maybe, I thought, I should resurrect that series.
I got to work. Sometime in September of 2018, I began making notes. My years of teaching screenwriting had turned me into a writer who thought in film terms, even for a novel. I wasn’t brainstorming, I was in pre-production. I wasn’t creating an outline, I was writing a treatment.
When final exams were over and the college closed for the holiday, I went to work. In what seemed like no time at all, I had 125 manuscript pages and it was feeling pretty good. In fact, I was encouraged and hopeful—two emotions I hadn’t experienced in a long time.
In early January, I was scheduled with my primary care provider for an annual physical. My PCP is a prince, a brilliant and caring physician whom I am personally fond of and trust absolutely. The physical went well. My blood pressure was under control; my off-the-chart cholesterol was finally within a normal range. Things were looking good. There was a smile on his face as we wrapped it all up.
“Wait,” I said, as I was about to hop down off the examining table. “I got something I want to ask you about. Give me your hand.”
He gave me the classic quizzical look, then held out his hand. I took it, flattened it out, then grabbed his index finger and put it against a spot on the left side of my neck, a few inches below my ear. I moved his finger around for a few seconds.
“What the hell is that?” I asked.
His brow furrowed. “I don’t know, but we’re going to find out.”
For months, I’d had this little knot on my neck, about the size of an English pea. It didn’t hurt. No discomfort at all.
It was just there.
Within a matter of days, I was sucked once again into the maw of the American health care medical/industrial complex. Ultrasound, CT scan, biopsy.
Non-Hodgkin’s lymphoma: blood cancer. It starts out in the lymphatic system and often manifests itself in swollen lymph nodes. My primary care provider set me up with an oncologist he’d worked with many times before. He was good, my doctor said, one of the best.
To top it off he was, like me, a pilot (although I hadn’t had the money to fly in nearly fifteen years). This assured him we’d have lots to talk about.
My third wife became an integral part of this process. Despite our difficulties, she’s one of the smartest people I’ve ever known. She starts researching lymphoma, especially my subset, which deploys frightening terms like “mantle cell” and “blastoid variant.” Apparently, my cancer is a very rare type, seen almost entirely in old white guys.
Years later, I would learn that it’s also tied to DNA. I don’t understand it, but apparently I have a few screwed up chromosomes.
The new novel gets set aside as it’s all I can do to teach my classes and attend to my treatments. I undergo a PET scan, which is an X-ray study where they inject you with radioactive sugar. Cancer cells love sugar; they’re voracious. When they slide you into the scanner, cancer cells light up.
My oncologist assured me that if I did what he told me to do and got with the program, he could cure me. The results of the PET scan, though, are not encouraging. I light up like Christmas at Rockefeller Center. My oncologist said they counted 36 tumors in my lungs. I never got a count on the rest of my body, but they were scattered everywhere, little bursts of light on an otherwise dark landscape.
Like fireworks, only on the inside.
I started an eight-week regimen of immunotherapy to shrink the tumors and get them under control. For me, immunotherapy was a cakewalk. I was able to drive myself to the treatment lab, get the infusion, then head to Watkins to teach my classes. About as close to a normal life as a cancer patient ever gets…
Hey, I thought, I got this.
Then it’s time to start the actual chemotherapy, which is a regimen called RCHOP—one letter for each of the five chemicals that make it up. RCHOP’s a witches brew of chemicals, steroids, a bunch of other stuff that sounds scary as hell.
This was when I learned that as sophisticated as cancer treatment has become in the past decades, it’s still based on the same principle: Poison the cancer, poison the patient. See which one taps out first.
This stuff is so toxic and powerful that they send you home with a regimen of corticosteroids to take for five days to keep you from melting down. You take five pills the first day, four the next, then wind it down until you take one last pill five days out.
I took that one last pill on a Sunday, a day when I was having lunch with my daughters. My older one’s driving now, so we meet at a restaurant. The food’s not very good; we decide not to go back. But it was still fun, with laughs and hugs and kisses all around and a generally fine day—the last one I’d have for a long time.
The next morning, I’m wiped out. I ache all over, have a disabling fever, so weak I can’t raise my head in bed. I feel like I’ve been pulled through a keyhole. My wife comes in to remind me I have a doctor’s appointment for my follow-up. I barely have the strength to tell her I’m too sick to go.
I’ve never felt like this. I’ve had flu before, bad flu. I was in bed for two weeks with it once and felt crappy for months afterward.
This is a whole new level.
On top of that, the surgeon had done a biopsy and removed a tumor out of my right armpit (the same surgeon has operated on me six times in the last few years; I told him if he spent any more time inside of me, I was going to ask for a commitment).
Now the incision site’s hot, angry, swollen and bloated. There’s a rainbow of colors that aren’t supposed to be there: red, green, purple, black. Everything but healthy pink. Streaks were starting to radiate out from my arm and shoulder.
My wife phoned the oncologist and told them I was too sick to make the appointment. The next day, I was even sicker and the colors were growing more pronounced. My wife took a cell phone picture and texted it to the nurse. Now they’re concerned. The third morning, she took more pictures and texted them to the oncologist’s office.
“Get him in here,” they instructed. “Now.”
She helped me dress and gave me a shoulder to lean on as I limped to her car. At the oncologist’s office, a tech draws blood out of the chemotherapy port in my chest.
My white blood count has crashed. A normal white blood cell count is between 4,000 and 11,000 cells per microliter of blood. The lab tests revealed mine had dropped below 750.
My immune system was shot and I was going septic.
My oncologist walks into the examining room after reviewing the lab results. “You’re going to the hospital,” he said. “We’ve already made the calls.”
“Can I go home, get my laptop and bathroom stuff and a change of clothes?”
My oncologist looked me straight in the eye. “You don’t have time.”
I’m not going to name the hospital the oncologist sent me to, primarily because I don’t relish fighting a libel suit. But from the get-go, I had a bad feeling. As sick as I was, they kept me sitting in a chair for a couple of hours. There weren’t many nurses around. A single nurse escorted me to my room, then left. My wife helped me change into the dreaded hospital gown and I climbed onto the bed, by now barely conscious. Hours went by. I vaguely remember someone bringing me a form to fill out for dinner and breakfast the following day. Eventually, there was an I.V. bag hung on the stand next to me and I guess they started some kind of antibiotic.
That evening, I encouraged my wife to go home. I was stable, kind of, and still hoped I was in good hands. By now, she was exhausted and stressed. Taking care of a cancer patient is among the most demanding forms of caregiving possible.
That night, I asked for something to help me sleep. They gave me an Ambien, which I’d been taking for years after my bypass. I drifted in and out. Life became a blur.
There were tests and sticks, blood draws and palpitations. On the third day, they rolled me down to the basement, where an in-house doctor I’d never met shot my armpit full of lidocaine and lanced the infected surgery site, which now resembled a huge boil.
This guy looked like an extra out of Paddy Chayefsky’s The Hospital. He struck me as a late middle-aged burnout case, maybe in recovery from booze or drugs. Like he’d lost his own practice or been kicked out of another, but had gone through rehab so he got his license back and a job as an on-call surgeon for a few years until he retired.
All I remember was that the lidocaine didn’t help much, and when this medieval barber lanced the wound, I was suddenly soaking wet. My hospital gown was drenched in blood and pus, as was the sheet on the gurney. It was over quickly and his assisting nurse, a young overweight woman with tattoos, sent for a tech to roll me back to my room.
Once there, they shifted me over to the bed and then left me lying there in the blood-and-pus soaked hospital gown (the wound continued to fester; weeks later my surgeon’s partner would do a proper repair and get it resolved).
Hours later, maybe even the next day (it’s all kind of a blur), the hospital gown was now dry and crunchy and stuck to my skin. It was starting to smell kind of gamy as well, or maybe it was me since no one ever came by to help me shower or clean up. I finally rang for a nurse, who seemed irritated at my call, and asked her to please bring me a clean gown. She disappeared for five minutes, came back, tossed a fresh gown on the bed, turned and left.
I stared at it, wondering how the hell I was going to make this work. Finally, using my I.V. pole like a crutch, I managed to roll into the bathroom, peel off the old gown, which by now had cemented itself to my side and back, and ease myself into the new one. My wife came by later and saw my bed, which resembled a crime scene, and raised hell with the nurses, who finally brought some clean sheets.
At some point, my primary care provider came by to check on me. I was so glad to see him I pulled myself out of bed and went over to shake his hand. Only I wound up collapsing into his arms and sobbing uncontrollably, my whole body quaking, shivering. I was a helpless, blubbering, sick shell of myself. I kept apologizing between sobs: I’m sorry… I’m so sorry…
He put his arms around me and held me up, told me how sorry he was, that no one should have to go through this. He patted my back and when I finally pulled away, there were tears in his eyes.
I had hit bottom.
I was in the hospital for either five or six days (like I said, it’s a blur) and on one of those days my oncologist came by.
He explained that no one can ever predict how a patient will react to chemotherapy. Some tolerate it pretty well; others don’t. So on the first treatment, just to set a baseline, they hit you with the Full Monty. Obviously, I fell into the demographic that didn’t handle it that well. He was going to adjust the dose and also extend the time between treatments.
They released me from the hospital and within a couple of days, I was back teaching my classes.
Maybe a month later, I went in for my second RCHOP treatment. This time it wasn’t fun, but it didn’t send me into a state of collapse. The steroids were the hardest part; the huge initial doses send you into a brain frenzy. No sleep and you can’t turn your brain off.
Years later, my cousin described her experience with steroids during cancer treatments: The neighbors called the house at 2 o’clock in the morning and asked my husband why I was out in the front lawn weeding the flower beds…
A year later, she died at sixty-three.
Weeks later, I went in for my third RCHOP treatment. My oncologist told me he wanted me to take six treatments, eight if I could tolerate them. This one wasn’t too bad either.
In late May, 2019, I took the fourth treatment and it decimated me. I have no idea why. Maybe it was the cumulative effect. My bloodwork had been terrible for months. I was anemic, had no immune system left, had shaved my head after losing most of my hair (my nephew bought me the Heisenberg hat from Breaking Bad, so at least there was a cool component to it all), and was struggling to hold 130 pounds.
I think I just gave out.
After the post-treatment steroids were taken, I was unable to drive. My wife had been taking me to appointments for awhile anyway. This time, however, I limped through the lobby of the medical plaza, got on the elevator up to the 7th floor, staggered down a hallway about twenty feet from my oncologist’s office, then leaned against a wall and slid to the floor. My wife ran and got a nurse; they rolled a wheelchair down the hall and helped me into it.
They drew blood out of the chemo port in my chest, ran it through the lab, and then my oncologist came into the examining room. By now, I’m too weak to sit up and am lying flat on the table.
“You’re done,” he said. “You can’t take any more. We’ll schedule a PET scan. If we get a good result, then we’ll move forward.”
“If not,” he added a moment later, “we have some very difficult decisions to make.”
A couple of weeks later, a Friday afternoon in June, the phone rang. It’s the nurse in charge of patient education, who also happens to be my oncologist’s wife. She puts me and my wife on the phone together.
“I know you have an appointment to come in and get the results of your PET scan,” she said. “But when we got the results, we couldn’t wait. You’re clean. Not a spot anywhere.”
I sat on the living room sofa, unsuccessfully struggling to keep my composure. Finally I broke down, sobbing.
It looked like I was going to live…
At the appointment, we reviewed the results in more detail. My doctor wanted me to take as many as eight treatments; four had nearly killed me. And yet, they worked. My doctor told me if I’d do six more months of immunotherapy, he could pretty much guarantee my chances of recurrence would drop to less than one in ten.
I agreed.
I was skeletal at this point, exhausted, felt like I’d aged a couple of decades. RCHOP does a mean tap dance on your kidneys. I was diagnosed with Stage III kidney disease. At Stage IV, you go on dialysis. I had a lot of healing to do. But I had the summer to get a good start on it. Six months of immunotherapy would take me to the end of 2019.
Then I’d be done with it.
December, 2019: Christmas is always difficult in failed blended families. Holidays are awkward, strained, with the conflicts escalating to an even higher level.
But I had the spring semester to look forward to. It looked to be a lucrative one, as I was now—in addition to teaching my full load at Watkins—teaching two adjunct classes in the Belmont University Motion Pictures program. It even looked like a mild winter, thanks to global warming.
At the end of January, 2020, it all imploded. The Watkins College of Art, which had been in continuous operation since 1885, announced it was closing its doors. Its academic programs would be absorbed by and would migrate to Belmont University.
Watkins as a distinct, unique institution, however, would cease to exist at the end of the spring semester. A 135-year-long ride (twenty-five of which I’d been on) was over.
A little over a month later, a series of tornados tore through East and Downtown Nashville, levelling homes and businesses, knocking power out all over town. The Watkins campus is spared, but there’s no power. We’re out for another ten days, then it was time for spring break.
In the middle of spring break, the Covid-19 lockdown Pearl Harbored everyone. I transitioned six classes at two colleges to Zoom calls in 48 hours, which included upgrading the WiFi in our house to handle the load.
The toughest years of our lives had just begun.
February, 2022: For some reason or other, I’m still on the right side of the dirt.
For the first year after Watkins closed, we were in pretty good financial shape. Watkins and Belmont made a deal: any faculty or staff member who stayed in their job until the college closure was complete received six more month’s salary. Under Tennessee law, when conditions are imposed on severance pay, it’s no longer severance pay.
Which meant I could apply for unemployment as well, something I’ve done only one other time in my entire life. I live in the American South, where pay scales are low and government support almost nonexistent. The Federal government, though, kicked in massive Covid subsidies. My weekly checks are a windfall. I pay down credit cards, take care of some deferred maintenance on the house.
I even hooked up with a local flight school and flew enough hours to get current again for the first time in two decades.
When the College closed and held its last commencement via Zoom in May, 2020, Belmont kept me on salary to do what’s called a teachout with two students who needed one class apiece to graduate. We did two independent studies via Zoom.
I only later figured out what this meant. When the College opened a Film School in August, 1995, I was actually the first faculty member hired. I was recruited to teach screenwriting as an adjunct, a part-timer. When they kept me past the College closing until August, 2020, it meant that I was the last one out the door.
I don’t know why that still feels so weird even to this day. It’s a loss I can’t quit grieving.
By the middle of 2021, though, the money was drying up. After I finished my summer semester, I went back to work on the new novel, the seventh in my Nashville P.I. series. I finished it in a couple months and sent the manuscript around to a few trusted writers and friends.
I broke it into two groups: published writers with a track record and readers who were familiar with the first six books.
I was staggered by the response. My trusted, highly perceptive writer friends felt very positive about the manuscript. Writers compulsively suggest revisions, though, and most of them were good.
The guidelines I gave my beta readers were simple. I didn’t ask them to proofread or copyedit, no deep-dive developmental editing. Just a few simple questions: 1) Did you enjoy the book? 2) Were you actually able to finish it? 3) Whatever I was asking you to buy into, were you able to do it? 4) Was there anything that jumped off the page that didn’t work, that pulled you out of the story?
Simple stuff, but highly revealing… One beta reader who had read all the books in the series said this new one was the best of the lot.
I was so encouraged by the reactions and feedback that I began to hold out hope I could get a traditional deal. The first six books were published by an imprint of Random House, Ballantine Books. My editor had long-since retired so I knew no one there.
I began searching for an agent. I follow the trades and the daily ezines that flood my inbox. I knew the right websites, where to do the real digging. I contacted other writers I knew and asked them for insight and, if they were willing, references.
Plus I had a couple of awards and a list of nominations. I’d made a few regional best-seller lists. My first published novel was a New York Times Notable Book. I had what I thought was some street cred.
I queried sixteen agents in the first round.
The results were shocking, even to a tough, grizzled old veteran like me. I was used to being disappointed by publishing, had decades behind me of struggling to publish and survive as a writer. For every pat on the back publishing gave me over the decades, it punched me in the nose and kicked me in the nuts a dozen times. My expectations were low, but even they were not met.
Ten agents never bothered to respond. I got a few boilerplate rejections. One agent told me that since the pandemic lockdown, she’d been inundated with queries. When she started getting 65-70 emails a day, she stopped taking them. It would take her months to get through the submissions that were already sitting on her desk.
Apparently, every sumbitch on the planet wrote a book during the lockdown.
Finally, I got a ping. I queried an agent whose name I recognized but couldn’t quite place. Turns out, we’d worked together before on a novel I published with Avon years earlier. The acquiring editor for the book quit her job and this agent—who was still an editor at this stage of her career—took over the final stages.
Publishers have a term—orphaned—which is what happens when the acquiring editor of a book leaves the house or changes jobs before your book is published. Someone is always assigned to take it over, but it’s usually the kiss of death for a book.
It was in my case. The book I thought would be my breakout suspense thriller went nowhere. I’ve got a couple hundred remaindered copies in the garage if anybody’s interested.
The editor-now-agent remembered me fondly and was eager to see the new book, along with anything else I had. I was excited, hopeful. I sent her the whole manuscript of the seventh Harry James Denton book, which I’d titled Fade Up From Black, along with a proposal for another suspense thriller and a pitch for a third project.
Radio silence for six months…
Finally, she called me one day. Calls from agents are generally good news; rejections are emailed.
The agent explained, though, that while she liked the book, the challenges to selling it were too great. The market was terrible; this was the seventh book in a series where the publisher didn’t own the first six; the suspense-thriller partial was strong but needed work.
Then she hit me with the blockbuster: I don’t know how old you are, she said, but I’m in my late fifties. And increasingly, I’m finding myself pitching to editors who are in their mid-twenties. They want a different kind of book than we’re used to—a dystopian, pessimistic, cynical voice full of doom and gloom.
“I just don’t know how to sell it,” she said.
It was the first time in my career anyone had ever intimated that I was too old.
So I went with the original plan to publish it under my own imprint, Spearhead Press, where I’d published my backlist and a few other titles.
I began getting Fade Up From Black: The Return of Harry James Denton ready for publication. The eBook is released in February 2022, with the print editions—hardcover and trade paperback—set to launch in March. Early reviews are great. Ann Patchett’s Nashville bookstore, Parnassus Books, graciously offered me a signing. I’m selling almost as many books now as I was when Ballantine published the originals back in the Nineties.
One late February morning, my wife walks into the kitchen as I’m pulling together a mug of coffee.
“You know,” I said. “I’ve been having this weird thing lately. Doesn’t hurt or anything, but I can’t help noticing it. I’ve been having trouble swallowing.”
She looks up. “Better tell your doctor,” she said.
I nodded. I had a routine blood draw coming up the following week.
At my doctor’s office, my prince of a primary care provider is wrapping up the paperwork when I tell him about the swallowing thing.
Everything in medicine is so specialized these days. I liken it to taking your car to the mechanic with a shaky back tire and the mechanic says “Oh, I only do front tires. If you got a back tire problem, ya’ gotta go see that guy over there.”
So when my primary care provider sent me to an ENT guy, that doctor spent about a half-hour interviewing me, then looked down my throat and saw nothing. He snaked a fiber optic cable down my nose and spotted nothing as well. He only goes as far down as your Adam’s apple.
After that, another guy takes over.
A week later, I’m at the gastroenterologist. He’s a nice enough fellow, concerned and careful. He tells me I need an upper endoscopy, which is where they knock you out, snake a camera down your throat, and see what’s going on.
I’ve been anesthetized so many times over the last few years that I see another procedure as a chance for a nice, long nap. Propofol’s great. Not to be indelicate, but I can see why Michael Jackson kept a gallon jug of it around the house.
So my wife drives me in to the surgical center and in short order, I’m down for my morning nap. Only when I wake up, the doctor’s not there. The nurse is there with my wife in the recovery booth and they both look stricken. The nurse turns away and starts folding stuff.
My wife—who God knows has been through enough at this point—said the news was not good. The doctor’s not a pathologist, so he can’t diagnose it. But he’s seen this many times in his career.
Esophageal cancer…
A few days later, the biopsies come back and my wife and I are, once again, in my oncologist’s office. It’s official now: squamous cell carcinoma of the esophagus.
I confess to my doctor I know nothing medically about esophageal cancer, but as a guy who’s taught film for nearly thirty years, I do know it’s what killed Humphrey Bogart. I’ve read enough biographies of Bogie to know it’s a pretty gruesome death.
We’ve got to get another PET scan scheduled, he explained, and fast. This cancer is aggressive, stubborn. We’ve got to find out if it’s metastasized anywhere else. If it’s localized, that’s one situation. If it’s gone beyond the esophageal wall, that’s an entirely different circumstance.
They fast track a PET scan—thank God Medicare doesn’t require pre-approval—and the results are back quickly. A short few days later, we’re back in the oncologist’s office reviewing the results, which are encouraging. The cancer appears to have invaded one lymph node, but doesn’t seem to have gotten very far. They stage it out as a toss-up between 2-A and 2-B.
It could be a lot worse.
Then my oncologist looks up, as if he’d almost forgotten to mention something. There’s another hot spot, he says, that we found in the scan, down in your left inguinal area. We’ll have to biopsy it, but I’m pretty sure your lymphoma’s back as well.
Two different cancers in two different places at the same time…
Is that even allowed? I ask.
The oncologist starts me on Rituxan—the same immunotherapy I was on my first time at the rodeo—to get the Non-Hodgkin’s lymphoma under control. No one seems too worried about that. The throat cancer is the first priority. In one of our early meetings, as the oncologist describes the nasty side effects of the radiation and chemotherapy I’ll have to endure, I stop him mid-sentence.
“Wait,” I interrupted. “I’m not saying I’m going to do this, but I’ve got to ask. What happens if I do nothing?”
The oncologist studies me for a few moments. “In two to three months,” he begins, “your esophagus will be completely closed off and you will begin the process of starving to death.
“At that point, we can insert a feeding tube, but by then it will be too late. The cancer will have metastasized. It will attack your liver first, then it will head for your lungs. Within four months, perhaps a little longer, you’ll be dead.”
I suddenly flash on Owen Wilson in Armageddon: “Okay, worst case scenario, I’ll be dead in four months… Let’s not go that route.”
The oncologist goes on to explain that the standard treatment for esophageal cancer—a chemotherapy identified by the acronym FLOT—is apparently more brutal than RCHOP. He admits that he’s seen many patients simply meltdown from the treatment.
“Well, we already know I don’t have a high tolerance,” I said. “Maybe start out baby steps?”
The oncologist nods. “Baby steps.”
Then we begin the discussion of radiation. I’ll be getting radiation and chemotherapy at the same time, which sounds disabling. Weeks earlier, I’d already started the eighth Harry James Denton novel. I’m not teaching anymore, so I’m determined to write this book while getting treatment.
I refuse to let this goddamn disease define me.
We’ve already consulted with the best esophageal surgeon in town, who declared my tumor inoperable. It’s too high up, too close to my windpipe. He can’t get good margins. I’ve done just enough research to know that an esophageal resection is a brutal surgery, with months of difficult recovery and lasting side effects, like possibly losing your voice and never being able to eat a normal meal again.
I don’t know whether to be scared or relieved that I can’t have the surgery.
Then the radiation issue comes up again. I tell one doctor I’ve heard horror stories about radiation.
“The reason you hear those horror stories,” he explains, “is that they’re all true.”
I ask about something I keep seeing on late night commercials on local TV. Something called proton therapy, which claims to be much easier on the patient and much less destructive to surrounding tissue. My oncologist is familiar with proton therapy, which is traditional X-ray radiation with everything stripped out but the protons.
“But I don’t know if it’s appropriate for your kind of cancer,” he said. “Why don’t we find out?”
So he whips out his mobile and dials the facility, which is in Franklin, Tennessee, an upscale community just south of Nashville. A phone consult later, he hangs up.
“You’re a perfect candidate,” he said. “They do a lot of esophageal cancers down there.”
So I have a consult with them, which is at a facility not unlike a Ritz-Carlton-type 5-star hotel. There’s a fireplace in the lobby and a snack bar, leather sofas and chairs, flat screen TV on the wall. The staff and doctors are all young, overwhelmingly white and well-groomed, handsome or pretty depending on gender. Their presentations are effective, their data and numbers impressive.
My wife’s not impressed. She grew up poor, hardscrabble poor, with a disabled single mother who was confined to a wheelchair. She doesn’t have a lot of patience with the rich, pampered, and privileged.
So to be fair, I have a consult with the traditional radiation folks as well. Their facility’s in the basement of a hospital, which you get to by navigating an underground parking lot that’s like a set from a cheap, indie horror movie. The waiting room’s cramped, painted cinderblock walls, plastic chairs. The air’s stale, musty. There’s a homeless, one-legged guy in a wheelchair over in the corner. I’m sitting next to the waste can. He rolls over to throw something away then, maskless, starts coughing all over me.
Okay, call me a privileged, white guy asshole, but I can’t imagine coming to this place every day to get my gullet roasted.
There’s only one problem, I later discover. The proton therapy is massively more expensive than the traditional therapy. Guess somebody’s got to pay for all that leather furniture.
“I can’t afford the co-pays,” I say to my oncologist. “I’ll have to dig into retirement.”
“Good,” he says. “Because if you don’t, you won’t have any retirement.”
In the meantime, I’m still working on the eighth Harry James Denton novel, which carries a working title of Not Fade Away. For years I’ve been intrigued by lines from pop songs that were considered harmless and cute in their day, but are now so patently offensive that it’s frightening. In this case, Buddy Holly’s song—with the lyrics I’m gonna tell you how it’s gonna be, you’re gonna give your love to me—is a stalker’s anthem.
I go with the proton therapy, despite their decision to not give me any financial aid and their insistence I sign a long promissory note and put up a wheelbarrow full of cash as a down payment. I now have a second car note, but only one car.
The radiation is administered every day and the chemotherapy has to accompany it, so now I have an infusion pump plugged into the port on my chest and hauled around on a shoulder strap 24/7. I go to my oncologist’s office early Monday morning to have it put in, then head back to downtown Nashville on Friday afternoon to have it removed.
It’s such a pain getting downtown on a Friday afternoon that I quickly talk the techs into teaching me how to remove it myself. The first time I took it out, I texted pictures to my family and my buddies with a note: Just performed my first medical procedure on myself. Next week I’m removing my gall bladder.
So the routine began. My days revolve around appointments at the radiation center. The techs who administer my treatments are all young, smart, friendly and reassuring. Very quickly, it begins to feel almost comfortable. The doctors are all amazed at how well I’m tolerating the treatments. I’m losing a little weight; it’s tough to eat when it hurts to swallow and chemotherapy kills your appetite. But as the radiation doctor in Franklin says, I’m skating through this.
Until the last seven or eight of the twenty-eight treatments…
There’s a visible radiation burn on my chest now. The chemotherapy is starting to zap me. Fatigue’s becoming a factor. Then as I approach the end of the treatment cycle, they give me the bad news—you actually feel worse when the treatments are over. The radiation and chemotherapy continue to work for weeks after the treatments are done. You’ll feel terrible afterward.
They were right.
The radiation facility has a ceremony for patients who successfully complete their treatments. They award you a certificate, make a speech, then you get to ring a big brass bell. My wife and stepdaughter go with me that day. Everyone says I look tired in the pictures…
A couple of weeks earlier, I felt like it was time to document some of this so I began the memoir you’re reading right now. I’m making good progress until I finish the treatments, then I crash hard. I wake up in the morning and the effort of brushing my teeth, cleaning myself up, getting dressed and making up my bed is exhausting. I drink coffee, do a little work, then eat lunch.
A three-hour nap follows. Then another nap after dinner. Then bedtime, with a hard nine-hour sleep.
It’s frustrating, but the oncologist tells me it’s perfectly normal; in fact, he said, I got off light. I was supposed to feel this bad from the beginning.
I continue limping along for a couple weeks, then it lightens up a bit. And now, here I am, back to work on this piece and the novel. After the treatments were done, we’ll wait two months for a PET scan and then see if any of this has worked. The wait is driving everyone but me nuts; I’m too tired to worry about it. I’ve been living with it too long.
Two long months later, I go in for yet another PET scan. We’re gobsmacked by the results: the esophageal cancer is gone. My oncologist apparently is having trouble believing this, so he schedules me for an esophageal ultrasound, which means I’ll get a nice long nap again while they run a camera down my throat and get eyes directly on it.
I came out of my propofol nap to a smiling doctor. He’s taken a few biopsies to make sure, but he can’t see anything down there. Later, I’ll see the pictures myself. The pictures that were taken first showed an ugly, bulbous inflamed mass in my throat that looked huge and really angry.
Now, it’s just… gone.
My oncologist will later call me an outlier; he’s seen this before, but it’s rare. When the results of the biopsied tissue come back, the news is even better. They deploy the term complete remission.
Then comes the bad news. On the roller coaster adventure that every cancer patient undergoes, there’s almost always a gotcha’ for every gimme. The esophageal cancer’s in complete remission.
But the lymphoma’s back with a vengeance. I’ve become “Rituxan resistant,” a term I never dreamed I’d hear. But apparently the immunotherapy isn’t working anymore, so my oncologist is going to ramp it up with two other drugs. Then yet another PET scan… Depending on those results, I may go into another regimen of chemotherapy, which he warns me in advance will be rough.
Oh, he adds, you’ll need to be on Keytruda for two full years, not the one year we originally thought.
My wife has been taking notes the whole time, with just an occasional question. It’s not like her to sit so quietly. She’s usually right there in the thick of it. Finally, when we’re about finished, she goes straight for the elephant in the middle of the room.
“If he goes through this, all the discomfort and the debilitation and the expense, what’s the prognosis?”
My oncologist sits quietly for a few moments.
“If everything goes well, then statistically speaking, he has about a 1-in-4 chance of surviving three years.”
So there it is. I’m still on this side of the dirt, but the struggle to stay there will be a marathon, not a sprint.
If disease is a metaphor, mine seems to fit the pattern precisely. If we’ve seen anything in the past few years, it’s that everything feels broken.
My marriage and family is broken; our societal family has come apart at the seams and we’re at each others throats.
My wife and I are both physically broken, our house a laundry list of deferred maintenance items. Our national infrastructure is in a shambles. We can’t keep our bridges and roads in repair, can’t keep the grocery shelves filled, our streets safe. It’s so hot out west, the power grid’s failing. The wood on my deck is so old it’s curled up and rotten and I can’t afford to replace it. The hot water valve on the washing machine failed and the machine is too old to be worth the repair cost. With the medical bills, we can’t afford a new one so my wife’s figured out how to get clothes clean in cold water.
So that’s what it’s come down to. I have two college degrees, nearly thirty years in academia, have published thirteen books in five languages, co-written two television movies, and can’t afford to replace a washing machine.
Welcome to the new American middle class.
We have the finest doctors, nurses, techs in the world. The American health care system can save your life, as it has mine, repeatedly. And in doing so, it sucks up everything around you. It saves your life, but can leave you with little left to live it.
When my oncologist wanted to start me on Keytruda, I told him I was hesitant because it costs almost $13,000 a treatment, with my 20 percent copay being cash I didn’t have.
“Steve,” he said, “I don’t want that to be the reason you don’t take Keytruda. Remember, 64% of all cancer patients declare bankruptcy.”
Great, I feel better…
Disease, as it turns out, is a wonderful metaphor for contemporary life in America. As Paddy Chayefsky wrote in one of my favorite movies, The Hospital, “There’s a certain splendor to it…”
September 2022: I have no idea why or how I’m still taking up space on this planet. The men in my family are known to have stubborn streaks; we’ve been driving wives crazy for generations. My wife says the devil’s not ready for me.
It’s as good an explanation as I can come up with.
I do know this much: if I survive this, the financial effect is going to be devastating. By the end of the year, if I’m still around, I’ll be trying to figure out how to pay as much as $40,000 in medical bills.
That’s for Year One.
So that’s where I’ll leave this. I start the new immunotherapy when I get back from a conference in Florida in September. After my next PET scan, I’ll know where I stand. I’ll either be on my way to managing this long term and continuing to have some kind of life or, to quote my oncologist, we have some very difficult decisions to make.
Meanwhile, il faut cultiver notre jardin. I’m getting off my ass and back to work. Those pages aren’t going to write themselves.